Technology has made urological care safer, more precise, and less invasive.
For instance, wireless, implantable devices like the RENOVA system use targeted nerve stimulation to calm the bladder — no medications or tubes are needed. In one study, 71% of patients saw at least a 50% drop in symptoms within six months when using these devices.
At Western Reserve Hospital, physicians see the same shift. “Urology has a pretty long track record of innovation,” says our urologist, Dr. Damian Garcher. “Robotics answered a pretty pressing question in urologic oncology [the study of cancers].”
Let’s understand how technology has changed urology treatments at Western Reserve for the better.
Key Takeaways
- Robot-assisted surgery has become the standard for many urologic conditions, including prostate cancer.
- Minimally invasive urology procedures allow same-day discharges, faster healing, and less pain.
- Innovations in imaging and artificial intelligence create advanced urology diagnostics.
- Procedures that once required hospital stays are now done in outpatient or office settings.
- Northeast Ohio patients have access to the latest urology technologies at Western Reserve Hospital.
An Overview of Recent Technological Advancements in Urology
Traditional urological surgeries were invasive, recovery-intensive, and less precise. Over the past two decades, urology has moved over to minimally invasive, high-tech alternatives powered by robotics, microtools, and smart sensors.
Here are some of the most exciting advancements:
- Robot-assisted prostate and bladder removal (e.g., using the Da Vinci robotic system) has become standard for urological cancers.
- High-definition, digital flexible ureteroscopy is now used for kidney and ureteral stones, which allows for fine control of scopes and lasers with less risk to surrounding structures.
- Laser energy has replaced many mechanical methods, especially for kidney and ureteral stones.
- The percutaneous nephrolithotomy (PNL) technique was once used for large kidney stones. It has been miniaturized into miniperc, microperc, and ultraminiperc. This means doctors now make extremely small incisions and use small tools to minimize recovery time. It's similar to laparoscopic surgery done on the abdomen.
- Ultrasound and near-infrared spectroscopy (NIRS) are used for noninvasive bladder monitoring.
Discover how advanced imaging and non-invasive procedures are improving urology care as we discuss them below.
The Rise of Robotic Surgery in Urology
Before the widespread use of robots, radical prostatectomy, the removal of the prostate gland, was considered the gold standard treatment for localized prostate cancer.
But it required open surgery and had a high risk of complications, particularly to the surrounding nerves that control continence and sexual function.
In Dr. Garcher’s words, “Radical prostatectomy... was very technically demanding because it is very difficult to get to the prostate’s location from an open approach, [but] robotics has greatly aided in reaching difficult to access places.”
Robotic systems like the Da Vinci surgical system introduced multi-arm control, jointed instruments, and a 3D camera. This helped surgeons see the site from all angles, making surgery more precise, less invasive, and safer.
In one study of over 1,000 patients, 95% were discharged within 24 hours after robotic prostate cancer treatment. Blood loss was lower, and operating times were shorter compared to standard techniques.
Urological Procedures That Benefit Most From Robotic Surgery
Several urologic surgeries now routinely use robotic assistance. It improves outcomes, decreases incontinence rates, and reduces hospitalizations, according to Dr. Garcher.
The most common include:
- Radical prostatectomy. Using a multi-arm robotic system helps surgeons work around delicate nerves responsible for bladder control and sexual function. This prevents complications like erectile dysfunction.
- Radical kidney surgery. Robotics helps surgeons preserve as much healthy tissue as possible while removing kidney tumors.
- Bladder cancer surgery. During cystectomy or bladder reconstruction, robotic arms provide access to deep pelvic areas that are difficult to reach through open surgery.
How Robotic Surgery Works: Step-By-Step
While each urological procedure varies, here's the typical process:
- Preparation. After receiving general anesthesia, you're peacefully asleep throughout the procedure.
- Positioning. Your body is positioned to give surgeons the best access, with gravity helping to move organs away from the surgical site.
- Access setup. Your abdomen is filled with carbon dioxide and small trocars. Trocars are thin tubes that act as gateways for instruments and are placed through tiny cuts in the skin.
- Robot connection. The robot is positioned and connected to these access points. Despite the name “robot,” it never operates independently. It's simply an extension of your surgeon's hands.
- Surgery. Your surgeon remains in complete control, using hand controls at a console to guide the instruments with better precision and 3D visualization.
- Completion. Once finished, the robot is disconnected, all instruments are removed, and the small incisions are closed.
The result? Smaller incisions, less pain, faster recovery, and shorter hospital stays than traditional surgery — all with your surgeon in control every step of the way.
Many patients are surprised to learn that “robotic surgery” doesn't mean a robot is performing their procedure. In reality, it's your trusted doctor using advanced technology that boosts their natural skills and precision.
Robotic vs. Traditional Surgery: What’s the Difference?
Robot-assisted surgery has the same goals as traditional surgery in healthcare — just with smaller incisions, greater precision, and a faster recovery.
Here’s how the two differ:
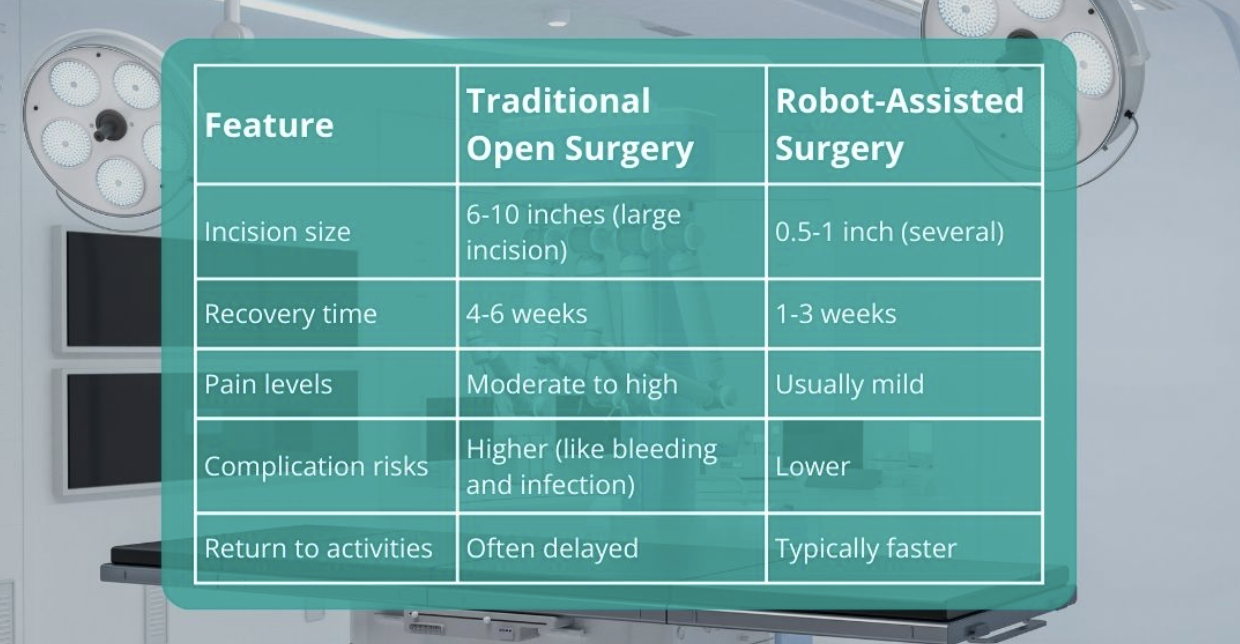
Because robotic tools operate through tiny incisions with extreme precision, they cause less trauma to healthy tissue. That’s why after minimally invasive urologic surgery, recovery tends to be smoother, with less pain and minimal scarring. Patients also return to normal activities sooner.
Clearing Up the Biggest Robotic Surgery Misconception
One common misconception is that the robot performs the surgery on its own. That’s not the case. As Dr. Garcher explains, “The robot is not doing the surgery... The surgeon is controlling it directly with their hands and fingers [at all times].”
As we’ve explained, the surgeon sits at a console and moves the robot’s arms with extreme precision, far beyond what human hands could do alone.
This means that while robots help surgeons see better, move more steadily, and reach hard-to-access areas, the surgeons remain fully in command at all times.
Imaging, Non-surgical Treatments, and the Future of Urology
Non-Surgical and Minimally Invasive Surgery Options in Urology
Not every urologic issue requires surgery (or robots). There are many alternative options for both cancerous and non-cancerous conditions, says Dr. Garcher.
Here are some of the most promising ones:
- Rezūm (steam therapy). This in-office procedure delivers controlled bursts of water vapor into excess prostate tissue. As the tissue shrinks over time, urinary flow improves.
- Aquablation (for enlarged prostate). This non-surgical benign prostatic hyperplasia (BPH) treatment uses real-time ultrasound and a robotically controlled water jet. It removes obstructive prostate tissue with high precision.
- iTind™ device. This is a temporary implantable stent that relieves urinary blockage without the irritation of a traditional catheter. It's placed and removed in the clinic.
- Laser kidney stone surgery. High-powered lasers are used to break apart kidney stones or remove small tumors with minimal damage to healthy tissue. Many cases are done under light sedation in outpatient settings.
Many of these treatments are done while patients are awake but comfortable, which allows them to go home the same day.
New Laser and Scope Technologies for Kidney Stones
Dr. Garcher says that laser and scope technologies for kidney stone treatments continue to improve. They now target difficult-to-reach stones with minimal disruption to surrounding tissue. The result is faster recovery and reduced need for repeat procedures.
Here are some examples:
- High-powered holmium lasers. They use controlled bursts of energy to break stones into fine particles. Surgeons can adjust energy levels and frequency to reduce heat, prevent stone movement, and shorten procedure time.
- Thulium fiber laser (TFL). This allows urologists to use smaller fiber tips (as small as 50 µm), which reduces the risk of tissue damage and provides better control.
- Flexible ureteroscopes. They have become smaller in diameter, some as thin as 7.5 French (just over 2mm). With slimmer scopes, urologists can access narrow areas without damaging the ureter.
- Single-use scopes. Reusable scopes demand careful handling and time-intensive sterilization. Single-use scopes avoid these issues while having similar performance in vision and maneuverability.
Advancements in Imaging and Diagnostic Tools
Urology imaging technology and diagnostic tools have also advanced. Here are some of the latest advancements:
- 3-Tesla MRI with spectroscopy and diffusion imaging. It gives detailed pictures of prostate and kidney tissue compared to older systems. This allows for earlier detection of suspicious lesions and more precise treatment planning.
- Contrast-enhanced ultrasound (CEUS). It has improved with safer contrast agents and clearer resolution. CEUS gives real-time images of blood flow in kidney or bladder masses without exposing patients to radiation. This prevents the harmful effects of radiation exposure.
- Elastography and 3D reconstruction. They now create more detailed, accurate maps of tissue stiffness and structure. This helps urologists distinguish between benign and malignant tissues with greater confidence and treat patients more effectively.
- MRI-guided biopsy. It has become more accurate by combining high-resolution MRI with live ultrasound, resulting in higher cancer detection rates. It also avoids unnecessary sampling of healthy tissue.
Artificial Intelligence in Urology
Artificial intelligence is everywhere, including urology. It helps urologists analyze complex data quickly and find patterns that would take much longer by hand.
AI models flag patients at higher risk for prostate cancer or kidney disease based on imaging, labs, and history. This helps urologists intervene earlier.
Algorithms also help match therapies to a patient’s tumor profile or response patterns, which means more effective, targeted treatment with fewer side effects.
What’s more, AI can track movements and anatomy in real time. This helps surgeons make quick and accurate decisions during delicate steps, especially when the margin of error is very low or visibility is limited.
Looking at the future, AI-based simulations show great potential for urological training. For example, AI systems could provide personalized feedback for surgical trainees learning complex urological procedures. It could also offer decision support during actual surgeries. Only time will tell how helpful these concepts are.
What’s Next in Urology: Looking Ahead 5-10 Years
Over the next decade, urology will continue moving toward greater precision, personalization, and less invasive care. Dr. Garcher also predicts that therapies will become even less invasive, leading to improved patient outcomes.
For example, surgeons may use augmented reality overlays during procedures to visualize internal anatomy, which could improve accuracy.
Similarly, targeted nanoparticles could deliver drugs or imaging agents directly to tumors. This is called nanomedicine, and it could reduce the impact on healthy tissue.
Future robotic platforms will likely also offer improved haptic feedback, smaller instruments, and better integration with imaging and AI.
How Urological Advancements Improve the Entire Experience
For patients, the benefits of modern urologic care go far beyond the operating room. Smaller incisions and minimally invasive options mean faster recovery, less postoperative pain, and fewer complications, says Dr. Garcher.
Many procedures now take place in outpatient settings, which reduces hospital stays and time away from work or family. This means lower disruption to your work life.
Follow-up care is often simpler, too, with fewer appointments and fewer disruptions.
Why Western Reserve Hospital Is Leading Urology Innovation in Northeast Ohio
Urology has changed dramatically over the past two decades. Surgical procedures are now more precise, imaging is clearer, diagnoses are faster, and recovery is easier on the body.
These changes come from steady, careful advances and tools that give surgeons better control and help patients heal with fewer setbacks.
At Western Reserve Hospital's Department of Urology, this progress shows up in the day-to-day care of our patients. Our urology team uses the latest minimally invasive urological surgery technologies to provide effective care to patients across Akron, Cleveland, and Northeast Ohio.
If you’re looking to understand your options, get a second opinion, or understand if newer treatments might be right for you, our team is here to help. You don’t have to go through it alone — book an appointment today.
Frequently Asked Questions
What Is Robot-Assisted Surgery in Urology?
Robot-assisted surgery is a type of surgery where a surgeon uses robotic tools to perform precise procedures through small incisions.
Is the Robot Performing the Surgery by Itself?
No. The surgeon controls the robot’s movements. The robot makes the surgery more precise, but it does not act independently.
What’s the Benefit of Minimally Invasive Procedures for Conditions Like Prostate Enlargement or Kidney Stones?
Minimally invasive procedures cause less pain, have quicker recovery, and often lead to better long-term outcomes.
Can I Be Awake for Procedures Like Rezūm or iTind™?
Yes. Many treatments can be done with sedation or local anesthesia in an office setting, depending on your needs.
