Why does pain feel different for everyone?
Some describe it as sharp and stabbing, while others label it as burning, aching, or impossible to explain. That’s because not all pain is the same.
In fact, there are three main types of pain: nociceptive, neuropathic, and nociplastic. Each type has a different cause and requires a different treatment.
To better understand these pain types, we spoke with Dr. Dmitri Souza, a nationally recognized pain specialist at Western Reserve Hospital.
Dr. Souza is board-certified in pain medicine, anesthesiology, internal medicine, and headache medicine. He has also authored more than 100 scientific publications, plus two books on pain and medicine.
In this article, he shares clear, practical insights to help patients understand their pain better and explore what treatment options work and why.
Key Takeaways
- Pain is not one-size-fits-all. It can be nociceptive, neuropathic, or nociplastic, and understanding which one you have is important for getting the right treatment.
- Nociceptive pain needs physical therapy and painkiller medications, neuropathic pain requires nerve-targeting meds, while nociplastic pain benefits from central modulation techniques.
- Western Reserve Hospital treats all types of pain with expert care. Our team uses a multidisciplinary approach to diagnose and personalize care for each patient’s unique pain experience.
What Are the Main Types of Pain?
Not all pain feels the same. A sharp jab, a dull ache, or an ongoing sensitivity that seems to have no clear cause are different types of pain. They come from different sources and need a different approach.
Let's break down the three main types of pain you should be aware of.
1. Nociceptive Pain
This is the most common type of pain. It happens when there’s actual damage to your body’s tissues, like the skin, muscles, joints, or internal organs.
Your body has special pain-sensing nerves called nociceptors. When tissue gets injured or inflamed, such as in the case of broken bones, it leads to activation of nociceptors. Activated nociceptors send signals to your brain saying, “Something’s wrong here!” That’s what causes the acute pain sensation you feel.
“Nociceptive pain results from tissue damage or inflammation and activation of peripheral pain receptors,” says Dr. Souza. It’s your body’s alarm system that tells you something is wrong and needs attention.
You’ve likely experienced nociceptive pain (or somatic pain) if you’ve ever had:
- A sprained ankle
- A surgical incision
- A dental procedure
- Osteoarthritis or rheumatoid arthritis
This type of pain tends to feel sharp, aching, throbbing, or tender, and it's usually located in a specific area. It also gets worse with movement and better with rest.
2. Neuropathic Pain 
Sometimes, when a nerve is injured or compressed, it starts firing off false alarms, even if there’s no soft tissue damage. These “misfiring” nerves send mixed or exaggerated messages to the brain, which interprets them as pain.
In other words, neuropathic pain comes from damaged or malfunctioning nerves, not from the skin, muscles, or joints themselves.
As Dr. Souza puts it, “Neuropathic pain arises from nerve damage as seen in diabetic neuropathy, post-herpetic neuralgia, or radiculopathy.”
Some common examples of medical conditions that lead to neuropathic pain include:
- Diabetic nerve pain
- Sciatica
- Shingles pain
- Carpal tunnel syndrome
- Trigeminal neuralgia
Because this pain originates in the nerves, it doesn’t usually respond to regular painkillers like ibuprofen. Treatments need to calm the nerves, often via medications like gabapentin or antidepressants that modify nerve signals. Neuromodulation can also be used to treat this type of pain.
3. Nociplastic Pain
Nociplastic pain is less known but very real. It arises when the central nervous system becomes hypersensitive to pain, even when there’s no active tissue damage or nerve injury.
According to Dr. Souza, nociceptive pain is commonly associated with fibromyalgia, post-stroke pain, and chronic psychogenic pain types. People with this type of pain feel ongoing, widespread discomfort and react strongly to even mild or harmless touch due to heightened sensitivity.
Nociplastic pain is also widespread and accompanied by fatigue, sleep disturbances, memory issues, or anxiety. Patients often feel misunderstood because their scans and lab results look normal. But the pain is very real; it’s a disorder of the pain processing system.
Unlike nociceptive or neuropathic pain, this type doesn’t respond well to standard painkillers or anti-inflammatories.
How to Tell the Difference Between Pain Types
The difference between the different types of pain is determined via patient symptoms, history, and diagnostic tests. Here is a quick breakdown: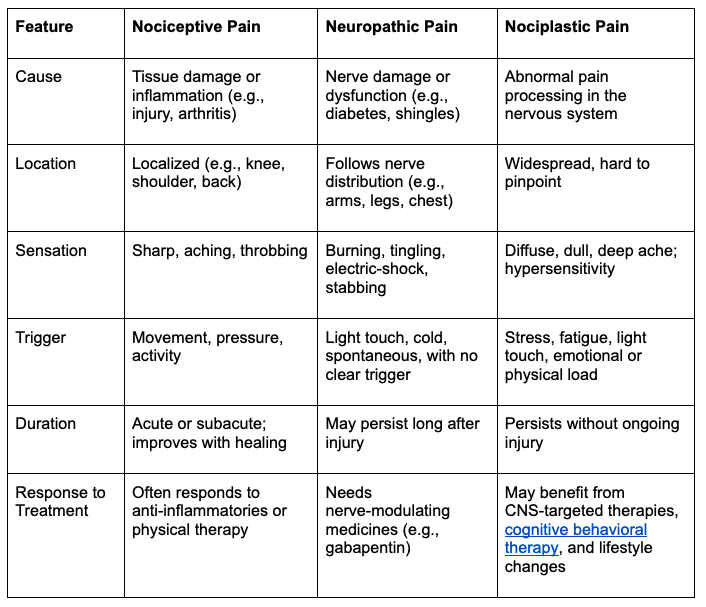
Key Symptoms to Look For
Your symptoms give healthcare providers clues about what kind of pain you’re dealing with.
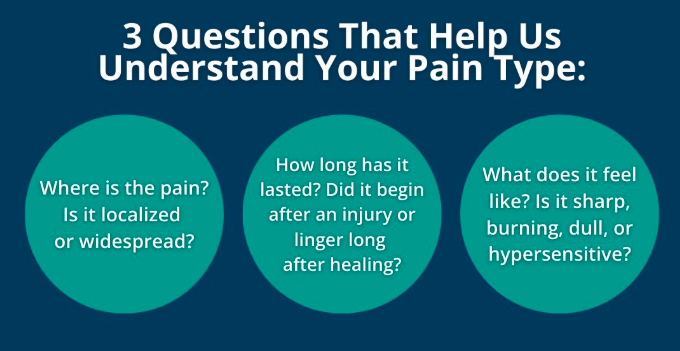
The three most important questions that help us understand your pain type are:
- Where is the pain? Is it localized or widespread?
- How long has it lasted? Did it begin after an injury or linger long after healing?
- What does it feel like? Is it sharp, burning, dull, or hypersensitive?
Importance of Patient History
Dr. Souza emphasizes that your own description of the pain is one of the most important diagnostic tools.
If you say the pain began with an injury and gets worse with movement, that points to nociceptive pain.
If you describe burning or electric shocks, we start to consider neuropathic pain. And if you say the pain lingers long after an injury has healed or is widespread without a clear cause, we start thinking about nociplastic pain.
According to Dr. Souza, if you accurately answer the following questions, it helps the doctors reach the right pain diagnosis:
- When and how did it start?
- What does it feel like?
- Does it come and go, or stay constant?
- What makes it better or worse?
- Have you had any past treatments? How did your pain respond to them?
- Do you also feel fatigue, poor sleep, brain fog, or mood changes?
Diagnostic Tools That Help
The foundation of diagnosis begins with a thorough history and clinical assessment. But additional diagnostic techniques help doctors distinguish between nociceptive, neuropathic, and nociplastic pain.
For example, Dr. Souza explains that a focused physical examination is crucial in evaluating pain. During the musculoskeletal physical exam, the physician assesses for patterns of tenderness, swelling, joint mobility, reflex changes, and sensory abnormalities.
Pain specialists also use diagnostic techniques like:
- MRI to detect herniated discs, nerve compression, or joint inflammation
- X-rays to see bone changes, like arthritis
- CT scans for more detail into deep tissue or spine issues
- Electromyography (EMG) and nerve conduction studies to evaluate how well your peripheral nerves are working. These are especially useful if you're feeling numbness, weakness, or tingling, which are all signs of neuropathic pain.
- Pain questionnaires like DN4, S-LANSS, or PainDETECT that screen for neuropathic components based on patient-reported symptoms.
In cases where pain diagnosis remains unclear, some more specialized testing can be used. For instance, skin biopsies assess small nerve fiber density in suspected small fiber neuropathy.
Quantitative sensory testing (QST) is another technique that evaluates sensory thresholds to identify hypersensitivity associated with nociplastic pain.
Why Pain Classification Matters for Treatment
When you're in pain, your first instinct is usually to find something — anything — that brings relief. But since different causes of pain behave differently in the body, their treatment differs greatly too.
Tailoring the Right Therapy
Understanding what type of pain you have determines whether your treatment will actually work. Dr. Souza puts it simply, “The classification of pain directly guides treatment selection.”
Your doctor needs to know what’s causing the pain at a biological level to know how to treat it effectively.
For example, nociceptive pain comes from tissue injury or inflammation. The goal of treatment for this pain type is to reduce that inflammation and support healing.
Neuropathic pain results from nerve damage or dysfunction, and common painkillers don’t help it. That’s because the problem isn’t inflammation, it’s misfiring nerves.
Nociplastic pain is even more complex. Traditional painkillers, including opioids, often fail because there’s no injury in the body. You need pain medications that work on brain chemistry to treat it.
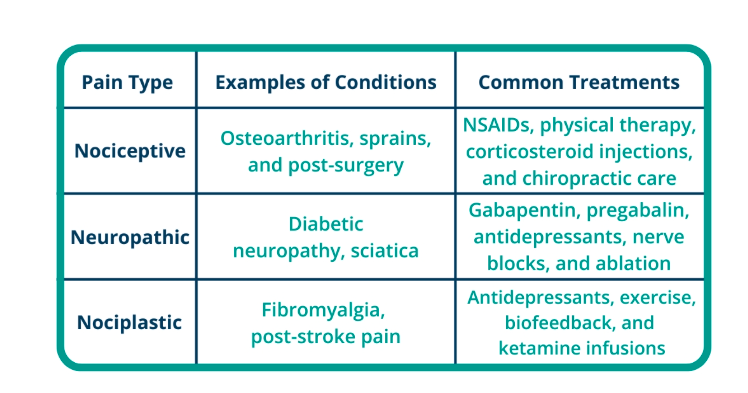
Examples of Targeted Treatments
Nociceptive pain is treated with medications that reduce inflammation, and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are the first-line in therapy. In some cases, steroid injections or physical therapy are added. If the pain is severe or post-surgical, short-term opioids may be considered.
Neuropathic pain requires medications that calm overactive nerve signals, like gabapentin or pregabalin. Certain antidepressants, such as amitriptyline or duloxetine, also stabilize nerve activity. For more targeted pain relief, your doctor may recommend nerve block or radiofrequency ablation to interrupt pain signals.
In fibromyalgia or post-stroke pain, the pain continues even after the original problem has healed (nociplastic pain). It can require low-dose antidepressants, exercise, therapy, biofeedback, and sometimes ketamine infusions to reset how the brain interprets pain.
Treating Mixed or Overlapping Pain Types
Pain doesn’t always fit into a single category. In fact, many people experience more than one type of pain at the same time.
You can have arthritis that causes nociceptive joint pain, while also dealing with sciatica, a form of neuropathic pain caused by nerve compression.
Similarly, you can have long-standing back pain that started with an injury but now includes nociplastic features like widespread sensitivity and poor sleep.
In such cases, doctors don’t rely on just one treatment method. Instead, they use a multimodal approach that combines different treatments. If you have knee arthritis and also sciatica, your care team will recommend NSAIDs or steroid injections for joint inflammation and add gabapentin or nerve blocks to manage nerve pain.
At the Center for Pain Medicine at Western Reserve Hospital, a full team works together to treat pain. Pain management doctors handle medications and injections, while physical therapists help with movement. Chiropractors offer manual therapy/acupuncture, and pain psychologists teach coping strategies like biofeedback.
Get High-Quality and Compassionate Pain Treatment at Western Reserve Hospital
Understanding pain classification and the type you’re experiencing is necessary to get the right treatment and lasting relief.
At Western Reserve Hospital, our team specializes in pinpointing pain types through detailed evaluations, advanced diagnostics, and a careful review of your symptoms and history.
Our approach combines medical expertise with leading-edge innovations such as regenerative therapies and minimally invasive procedures that stimulate healing and reduce downtime. We also integrate physical therapy, chiropractic care, and pain psychology into our plans.
You’ll receive compassionate, multidisciplinary care designed around your unique needs.
If pain is affecting your quality of life or mental health and current treatments haven’t helped, visit our website to schedule a consultation today.
FAQs About the Types of Pain
Can one person have all three types of pain?
Yes, a person can experience all three pain types in chronic or complex health conditions like fibromyalgia with past injury and nerve damage. Each type needs its own targeted treatment for effective relief.
How do doctors know what kind of pain I have?
Doctors identify your pain type through a detailed medical history, physical examination, and diagnostic tools like MRIs, EMGs, and pain questionnaires.
What if pain treatments aren’t working?
If your treatment is not working, it could mean the pain type was misidentified. Doctors will need to reassess your diagnosis, use different tests, and adjust your treatment plan.
